Medical Disclaimer: This article provides educational information about sleep disorders. Always consult with healthcare professionals for proper diagnosis and treatment of medical conditions.
Understanding Sleep Disorders
Sleep disorders affect millions of people worldwide and can significantly impact quality of life, health, and daily functioning. The American Sleep Association estimates that 50-70 million adults in the US have a sleep disorder, with many cases remaining undiagnosed and untreated.
Sleep disorders encompass a wide range of conditions that disrupt normal sleep patterns, from difficulty falling asleep to breathing interruptions during sleep. Early recognition and proper management can dramatically improve both sleep quality and overall health outcomes.
Important Statistics: Untreated sleep disorders increase the risk of cardiovascular disease by 40%, diabetes by 30%, and are associated with reduced life expectancy. However, most sleep disorders are highly treatable when properly diagnosed.
Insomnia: The Most Common Sleep Disorder
Insomnia affects approximately 30% of adults and is characterized by difficulty falling asleep, staying asleep, or waking up too early. It can be acute (short-term) or chronic (lasting more than 3 months).
Types of Insomnia
- Sleep Onset Insomnia: Difficulty falling asleep within 30 minutes of bedtime
- Sleep Maintenance Insomnia: Frequent awakenings or inability to return to sleep
- Early Morning Awakening: Waking up too early and unable to fall back asleep
- Mixed Insomnia: Combination of multiple insomnia types
Common Causes of Insomnia
- Stress and Anxiety: Work pressure, relationship issues, financial concerns
- Medical Conditions: Chronic pain, acid reflux, thyroid disorders
- Medications: Stimulants, antidepressants, blood pressure medications
- Lifestyle Factors: Irregular sleep schedule, excessive caffeine, screen time before bed
- Environmental Issues: Noise, light, uncomfortable temperature
Insomnia Management Strategies
- Cognitive Behavioral Therapy for Insomnia (CBT-I): Gold standard treatment addressing thoughts and behaviors
- Sleep Restriction Therapy: Limiting time in bed to actual sleep time
- Stimulus Control: Associating bed and bedroom with sleep only
- Relaxation Techniques: Progressive muscle relaxation, meditation, breathing exercises
- Sleep Hygiene Optimization: Consistent schedule, optimal environment, pre-sleep routine
Sleep Apnea: The Silent Epidemic
Sleep apnea is a serious disorder where breathing repeatedly stops and starts during sleep. It affects an estimated 22 million Americans, with 80% of moderate to severe cases remaining undiagnosed.
Types of Sleep Apnea
- Obstructive Sleep Apnea (OSA): Most common type caused by airway blockage
- Central Sleep Apnea: Brain fails to send proper signals to breathing muscles
- Complex Sleep Apnea: Combination of obstructive and central sleep apnea
Sleep Apnea Symptoms
- Nighttime Symptoms: Loud snoring, gasping, choking, frequent awakenings
- Daytime Symptoms: Excessive sleepiness, morning headaches, difficulty concentrating
- Mood Changes: Irritability, depression, anxiety
- Physical Signs: High blood pressure, weight gain, decreased libido
Sleep Apnea Risk Factors
- Physical Factors: Obesity, large neck circumference, narrow airway
- Demographics: Male gender, age over 40, family history
- Lifestyle: Smoking, alcohol consumption, sedentary behavior
- Medical Conditions: Diabetes, heart disease, stroke history
Sleep Apnea Treatment Options
- CPAP Therapy: Continuous positive airway pressure to keep airways open
- Oral Appliances: Custom devices to reposition jaw and tongue
- Lifestyle Changes: Weight loss, exercise, sleep position modification
- Surgical Options: UPPP, maxillomandibular advancement, inspire therapy
Health Impact: Untreated sleep apnea increases the risk of heart attack by 30%, stroke by 60%, and is associated with a 3x higher risk of motor vehicle accidents due to daytime sleepiness.
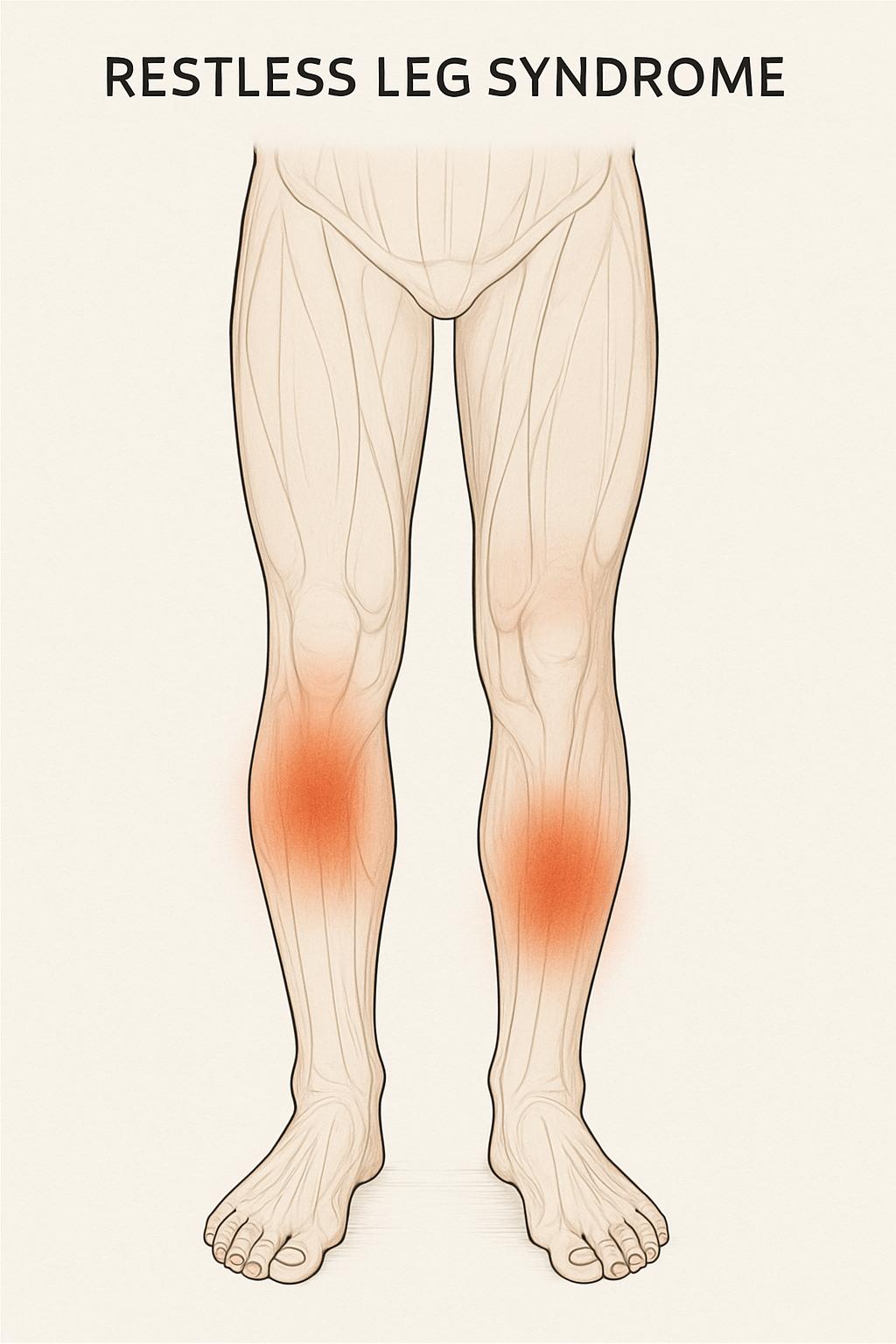
Restless Leg Syndrome (RLS)
RLS is a neurological disorder characterized by uncomfortable sensations in the legs and an irresistible urge to move them, typically occurring in the evening or at night.
RLS Symptoms
- Uncomfortable Sensations: Crawling, tingling, burning, or aching in legs
- Urge to Move: Irresistible need to move legs to relieve discomfort
- Evening Worsening: Symptoms typically worsen in the evening or at night
- Movement Relief: Symptoms temporarily improve with movement
- Sleep Disruption: Difficulty falling asleep due to leg discomfort
RLS Management
- Iron Supplementation: Address iron deficiency if present
- Lifestyle Modifications: Regular exercise, leg massages, warm baths
- Trigger Avoidance: Limit caffeine, alcohol, and certain medications
- Medications: Dopamine agonists, anticonvulsants, opioids for severe cases
Narcolepsy: Excessive Daytime Sleepiness
Narcolepsy is a chronic neurological disorder that affects the brain's ability to regulate sleep-wake cycles, leading to excessive daytime sleepiness and sudden sleep attacks.
Narcolepsy Symptoms
- Excessive Daytime Sleepiness: Overwhelming urge to sleep during the day
- Cataplexy: Sudden muscle weakness triggered by emotions (Type 1 narcolepsy)
- Sleep Paralysis: Temporary inability to move when falling asleep or waking up
- Hypnagogic Hallucinations: Vivid, dreamlike experiences during sleep transitions
- Fragmented Nighttime Sleep: Frequent awakenings and poor sleep quality
Narcolepsy Management
- Stimulant Medications: Modafinil, armodafinil, methylphenidate
- Antidepressants: For cataplexy and REM sleep symptoms
- Sodium Oxybate: For nighttime sleep consolidation and daytime symptoms
- Lifestyle Strategies: Scheduled naps, consistent sleep schedule, safety precautions
Circadian Rhythm Sleep Disorders
These disorders involve disruptions to the internal body clock, causing sleep to occur at inappropriate times relative to conventional sleep-wake schedules.
Types of Circadian Rhythm Disorders
- Delayed Sleep Phase Disorder: Sleep and wake times are significantly later than desired
- Advanced Sleep Phase Disorder: Sleep and wake times are significantly earlier than desired
- Shift Work Sleep Disorder: Difficulty adjusting to work schedules that conflict with natural circadian rhythm
- Jet Lag Disorder: Temporary misalignment due to rapid travel across time zones
Treatment Approaches
- Light Therapy: Strategic bright light exposure to shift circadian phase
- Melatonin Supplementation: Timed melatonin to promote phase shifts
- Chronotherapy: Gradual adjustment of sleep schedule
- Sleep Hygiene: Consistent sleep environment and routines
Parasomnias: Abnormal Sleep Behaviors
Parasomnias are disruptive sleep-related disorders involving abnormal movements, behaviors, emotions, perceptions, or dreams during sleep transitions.
Common Parasomnias
- Sleepwalking: Complex behaviors performed while asleep
- Sleep Terrors: Episodes of intense fear and panic during sleep
- REM Sleep Behavior Disorder: Acting out dreams due to lack of muscle paralysis
- Sleep Eating Disorder: Eating episodes during partial awakening from sleep
- Nightmare Disorder: Frequent disturbing dreams that cause distress
Parasomnia Management
- Safety Measures: Secure environment to prevent injury
- Trigger Identification: Address stress, medications, or other triggers
- Sleep Hygiene: Consistent schedule and adequate sleep duration
- Medications: Clonazepam, melatonin, or other specific treatments
When to Seek Professional Help
Knowing when to consult a healthcare provider or sleep specialist is crucial for proper diagnosis and treatment of sleep disorders.
Red Flag Symptoms
- Chronic Insomnia: Sleep problems lasting more than 3 months
- Loud Snoring: Especially with gasping or choking sounds
- Excessive Daytime Sleepiness: Falling asleep during daily activities
- Unusual Sleep Behaviors: Sleepwalking, acting out dreams, or sleep eating
- Morning Symptoms: Headaches, dry mouth, or unrefreshing sleep
- Mood Changes: Depression, anxiety, or irritability related to sleep
Sleep Study Evaluation
- Polysomnography: Comprehensive overnight sleep study in a lab
- Home Sleep Tests: Simplified testing for sleep apnea screening
- Multiple Sleep Latency Test: Assessment of daytime sleepiness and narcolepsy
- Actigraphy: Wrist-worn device to monitor sleep-wake patterns
Living with Sleep Disorders
Managing a sleep disorder requires ongoing attention and often lifestyle adjustments, but with proper treatment, most people can achieve significant improvement in their sleep and overall health.
Long-term Management Strategies
- Treatment Compliance: Consistent use of prescribed therapies (CPAP, medications)
- Regular Monitoring: Follow-up appointments and sleep study updates
- Lifestyle Optimization: Weight management, exercise, stress reduction
- Support Systems: Family education, support groups, sleep disorder communities
- Technology Utilization: Sleep tracking apps, smart CPAP machines, telemedicine
Quality of Life Improvements
- Better concentration and cognitive function
- Improved mood and emotional stability
- Enhanced physical health and energy levels
- Reduced risk of accidents and injuries
- Better relationships and social functioning
- Increased work productivity and performance